
Health Care & Wellness
Alcohol Legislation Takes A New Turn: Canned Cocktails, Direct-to-Consumer Shipping, and More
February 12, 2026 | Kerrie Zabala
October 8, 2025 | Abbie Telgenhof, Morgan Scarboro
-000055-1200px.jpeg)
Key Takeaways:
H.R. 1, also known as the One Big Beautiful Bill Act (OBBBA), was signed into law by President Trump on July 4, 2025. The bill’s healthcare, tax, and spending priorities will have a significant impact on states. We anticipate that most states will address these changes in 2026 or beyond.
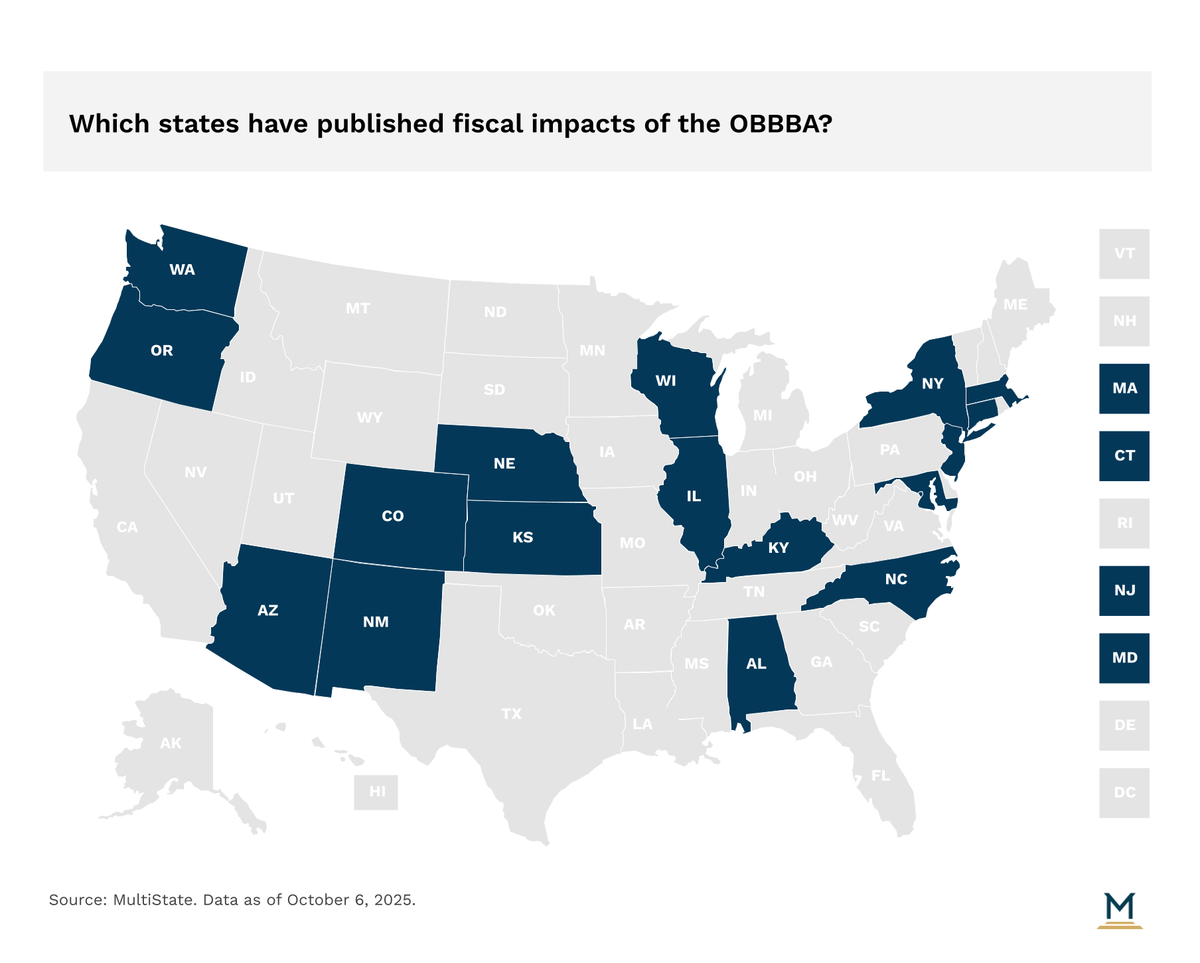
In preparation for these discussions, nearly twenty states (primarily democratically controlled states) have published various analyses on the impacts that OBBBA will have on their state. Some of these reports are more partisan in nature, while others are more fiscally focused, but they all provide a preview of states’ priorities in upcoming sessions.
Changes to the Supplemental Nutrition Assistance Program (SNAP) will have significant cost implications for states. Previously, the federal government funded all of the benefit costs and split the administrative costs with states. However, beginning next year, states will begin paying 75% of administrative costs, and, beginning in 2027, states will be responsible for a portion of the benefit costs — up to 15% depending on states’ error rates. Even without accounting for increased administrative costs, the benefit-cost shift could cost states hundreds of millions per year if states decide to continue funding the program at its current level. Although policymakers will need to address these funding questions, they have some time to consider options and funding mechanisms as these changes will take several years to phase in.
OBBBA marks the most sweeping change to Medicaid and coverage policy since the enactment of the Affordable Care Act. Specifically, six provisions will have the largest influence on states’ budgets by reducing federal funding by more than $792 billion over 10 years. These provisions include work requirements, provider tax rates, state-directed payments, six-month redeterminations, uniform tax waivers, and Emergency Medicaid's Federal Medical Assistance Percentage (FMAP).
The heaviest lift for states in the short term is not fiscal in nature but administrative. Beginning in January 2027, states will be required to implement and ensure Medicaid expansion enrollees comply with both work requirements and six-month verification processes. Implementing work requirements has proven to be an administratively complex process, as illustrated by experiences in Georgia and Arkansas. Simultaneously, performing six-month eligibility verification procedures is likely to require increased administrative personnel to accommodate the increased onus on agencies. An inability to invest in personnel and resources at the state level to handle the increased workflow may result in higher processing errors or churn rates, creating procedural disenrollments (i.e., enrollees lose coverage not due to eligibility but because of paperwork or administrative issues).
The loss of federal Medicaid revenue over the next ten years, if implemented as enacted, would be near impossible for individual states to make up the difference on their own. However, when the U.S. Senate passed its final version of the reconciliation bill, it also accommodated for effective dates that mitigate fiscal implications for states in 2025 and 2026. Based on the six key Medicaid provisions in the bill, states won’t realize the most drastic cuts in federal Medicaid revenue until 2028 at the earliest. Notably, between 2025 and 2027, only 6% of the $792 billion in cuts from the six largest Medicaid provisions will hit state budgets.
The MultiState team has been compiling the state-specific impacts of the One Big Beautiful Bill. Nearly twenty states have published reports or directed agencies to respond, and it’s likely that more will follow. To access our state-by-state report, please reach out to us here. We will continue to update this analysis throughout the remainder of the year as more states respond to the OBBBA and its impacts.

February 12, 2026 | Kerrie Zabala

February 5, 2026 | Geoff Hawkins

February 4, 2026 | Morgan Scarboro