
Health Care & Wellness
State Tobacco Legislation in 2025 Tackled Vaping, Nicotine Pouches, and More
February 5, 2026 | Geoff Hawkins
August 7, 2025 | Lisa Kimbrough

Key Takeaways:
For several years, states have been actively curbing the operations of pharmacy benefit managers (PBMs). Legislators have pursued various approaches to PBM reform, including prohibiting gag clauses in pharmacy contracts and imposing numerous reporting obligations. The latest reform strategies are extensive, focusing on rebate pass-throughs, delinking, fiduciary duty, and pharmacy ownership.
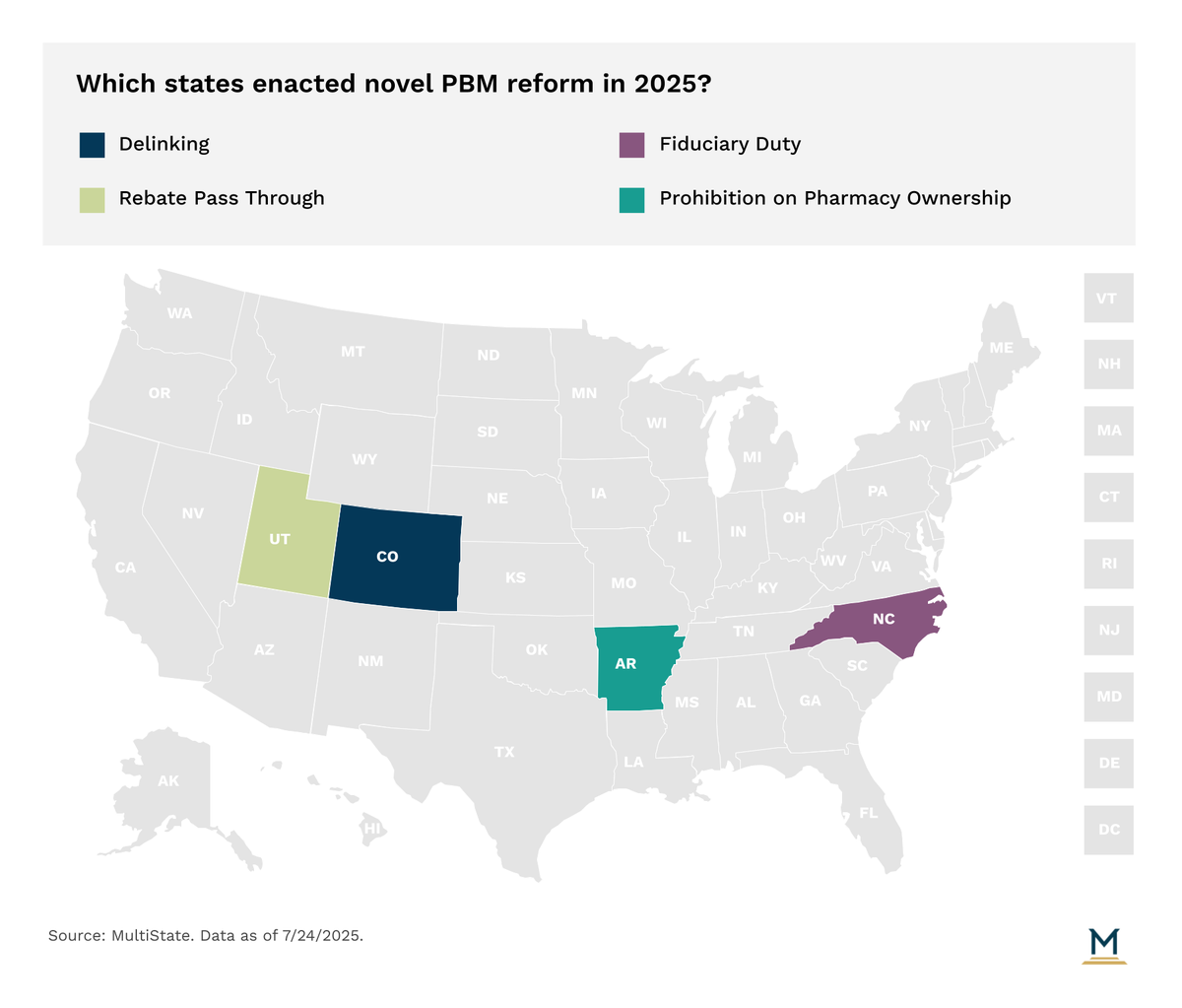
Instead of basing PBM compensation on rebates and discounts negotiated with drug manufacturers or the list prices of drugs, delinking would mandate that PBMs receive flat, fixed fees for their services. This price structure would “delink” the price of the drugs from the PBMs’ profit, thus removing incentives for PBMs to charge higher prices for prescriptions. Colorado is the only state that has adopted such a reform. It takes effect January 1, 2027.
Manufacturers offer rebates for the purchase of their pharmaceuticals, but it can get a little complicated when the end user of the product did not purchase it directly from the manufacturer. PBMs earn millions of dollars by keeping the rebates on drugs they get from the manufacturer. Utah adopted a bill that requires health insurers to make sure their PBMs either pass the rebate on to the consumer at the point of sale, use the rebates to reduce premiums of the enrollee, or increase benefits for the enrollee.
Fiduciary duty is a relatively new concept to the world of PBMs. These bills ensure that the PBM acts as the health carrier’s agent and owes a fiduciary duty to the carrier with relation to prescription drug benefits. Prior to this year, only two states (Maine and Vermont) mandated that PBMs owe a fiduciary duty to the health carrier. North Carolina’s major PBMs reform bill added this provision to PBM requirements this year.
This year, the most significant news in pharmacy benefit manager (PBM) reform is Arkansas's new law prohibiting PBMs from owning pharmacies. While similar measures in Indiana and Louisiana were ultimately removed from their respective bills, Arkansas's prohibition was enacted. However, the law has not yet taken effect due to immediate legal challenges.
StateVitals is the leading resource on how state governments are shaping healthcare policy and transforming care and delivery, brought to you by MultiState’s Health Care Policy Practice. MultiState’s policy and advocacy professionals are uniquely positioned to give you and your organization the big-picture view on state health policy reform, plus the latest trends on how policymakers are thinking about healthcare and similar emerging issues. Learn more about StateVitals, or schedule a demo here.

February 5, 2026 | Geoff Hawkins

January 27, 2026 | Lisa Kimbrough

January 27, 2026 | Amber Thyson