Key Takeaways:
- Prior authorization reform is accelerating through multiple legislative strategies, including gold card programs that allow high-approval providers to bypass requirements, removal of authorization for specific drug classes, and mandatory decision timeframes for urgent and non-urgent requests.
- Gold card programs are expanding and evolving, with Arkansas, Texas, and West Virginia amending existing programs to extend privileges to group practices, increase look-back periods, and refine coverage categories during the 2025 legislative session.
- Artificial intelligence restrictions are emerging as a new focus area, with states like Maryland requiring patient-specific rather than group datasets for AI-driven decisions and mandating reporting when AI contributes to adverse determinations.
- Continuity of care provisions are gaining traction, with multiple states requiring new health plans to honor prior authorizations from previous insurers for 90 days to one year, particularly for chronic conditions and rare diseases.
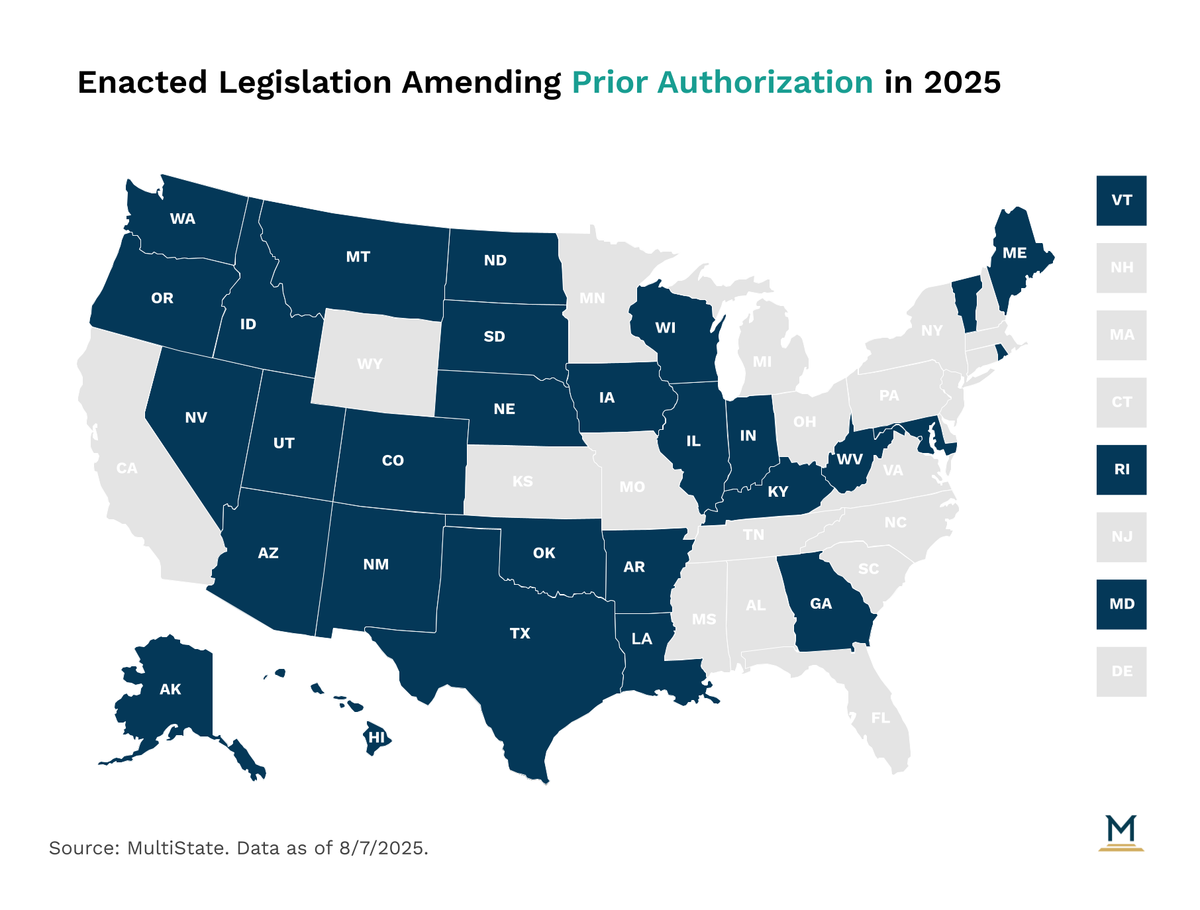
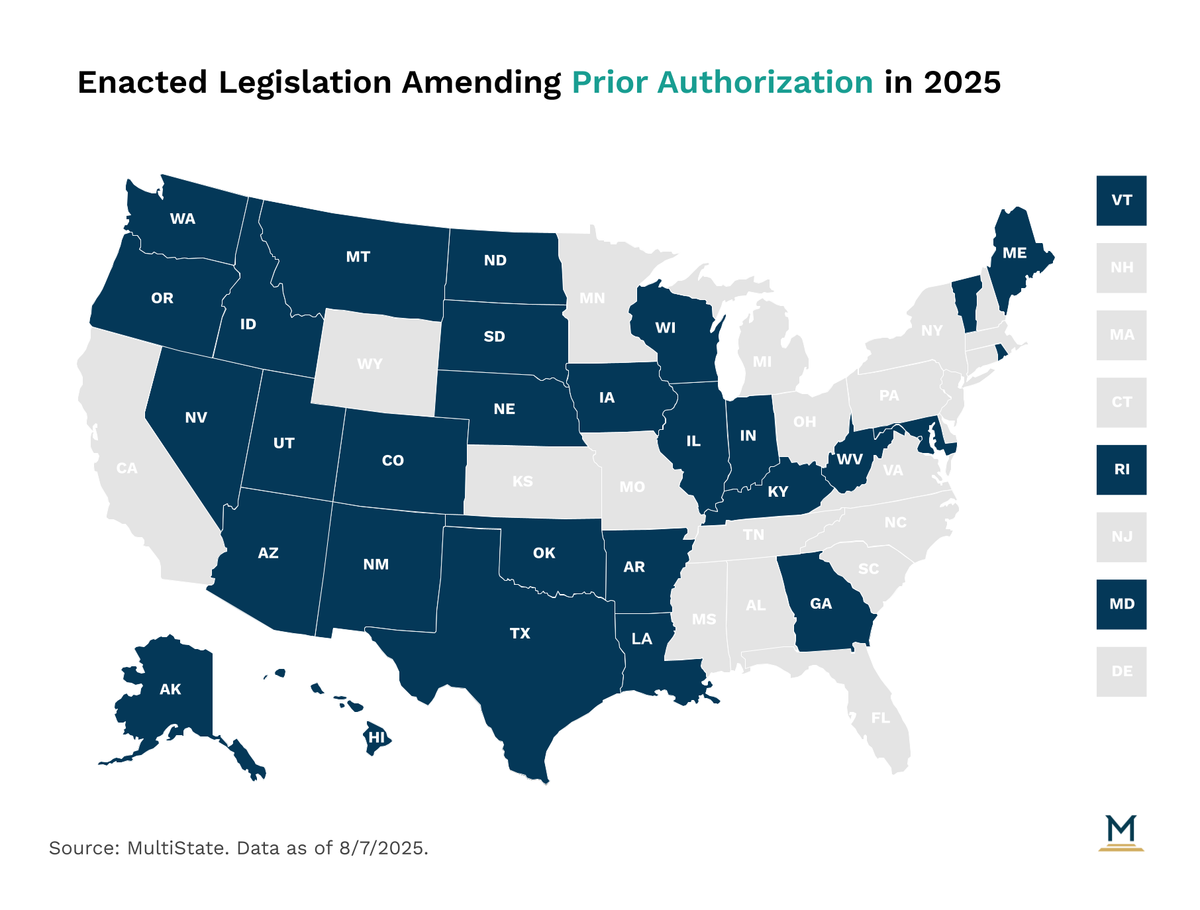
Prior authorization has been a recent target of legislative activity to increase patient access. One method of reducing prior authorization is “gold carding”, but states have also pursued a handful of other tools.
Prior Authorization Reform Trends in 2025
Gold Card Programs Lead Prior Authorization Reform
Gold carding instructs insurers to allow providers who have a high (80%-90%) prior authorization approval rate to bypass prior authorization for up to a year for those prescriptions or services they routinely get approved for. Arkansas, Colorado, Louisiana, Texas, West Virginia and Wyoming have all adopted gold carding legislation prior to this past legislative session. In 2025, Arkansas, Texas and West Virginia amended their existing gold card programs.
Other Ways to Increase Patient Access
Another path to increase patient access is removing prior authorization or step therapy altogether for specific classes of prescription drugs or procedures. This is most commonly seen with drugs prescribed for mental health or cancer. Similarly, there was a trend to extend prior authorization granted by one insurer to an enrollee’s new policy for a specified amount of time, generally 3 months to a year. Also, requiring insurers to make determinations within 24 hours for urgent requests or 48 hours for non-urgent requests.
Artificial Intelligence Restrictions Emerge as New Focus
Lastly, a handful of bills prohibited the use of AI in prior authorizations, or to require confirmation of adverse prior authorization decisions from a human medical professional, and to provide transparency for denials.
Notable Prior Authorization Enacted Legislation in 2025
Below are a few notable bills that addressed prior authorization during the 2025 state legislative sessions.
- Arkansas: HB 1301 amends the state’s gold card program to remove the existing allowance for insurers to withdraw gold card status from a healthcare provider if that provider increases the number of gold carded procedures by 25%. It also extends the gold card privilege to the provider’s group practice.
- Iowa: HF 303 requires utilization review organizations to provide decisions within specific timeframes, for, urgent requests within 48 hours of receipt and for non-urgent requests within 10 calendar days. It also requires utilization review organizations to submit annual reports to the Insurance Commissioner, including the data on approval/denial rates for both urgent and non-urgent requests. The bill originally included a gold card pilot program, but that was removed at the last minute.
- Indiana: SB 480 establishes timeframes for review of prior authorizations. Urgent requests must be reviewed within 24 hours and non-urgent requests must be reviewed within 48 hours. It also requires a utilization review entity to honor an authorization that was granted to a covered individual by a previous utilization review entity for at least the initial 90 days of the covered individual's coverage under a new health plan.
- Maryland: HB 820 mandates that insurers using artificial intelligence for utilization review do not allow the use of group datasets for decision making, but patient-specific information. The insurer must also report to the Insurance Commissioner if artificial intelligence was used in any adverse determinations.
- Montana: HB 398 requires that when a person switches health plans, the new plan must honor prior approvals for healthcare services for at least three months. It further establishes that only licensed physicians can issue adverse determinations. The bill also makes prior authorization approvals valid for 12 months for enrollees diagnosed with chronic conditions.
- New Mexico: HB 39 removes prior authorization and step therapy for enrollees diagnosed with rare disease. It includes off-label prescribing in that exception, if the medication is being used for the treatment of a rare disease.
- Texas: HB 3812 extends the gold card look-back period from 6 months to one year.
- West Virginia: SB 833 removes the prescribing of medication from the gold card program.
Track Health Care Policy with State Vitals
StateVitals is the leading resource on how state governments are shaping healthcare policy and transforming care and delivery, brought to you by MultiState’s Health Care Policy Practice. MultiState’s policy and advocacy professionals are uniquely positioned to give you and your organization the big-picture view on state health policy reform, plus the latest trends on how policymakers are thinking about healthcare and similar emerging issues. Learn more about StateVitals, or schedule a demo here.